Jump to
Stability and clinical anatomy
Admission, discharge and calling a senior
Overview
Ankle fractures are one of most common adult fracture types seen worldwide. The majority will be managed and sent home by the emergency department (ED).
The fractures that you will be referred are:
- Unstable fractures that need clerking/admitting for surgery (often fracture dislocations that have been reduced by ED)
- Open fractures (make sure your hospital admits open fractures or whether they get sent straight to a trauma centre from ED). For more on open fractures, see here and here
- Fractures where the reduction has been unsuccessful or the ED are unwilling to attempt reduction (e.g. patient unfit for sedation)
- Simple fractures where the patient has failed a mobility or physio assessment and are unsafe to go home (social admissions – important to check your hospital policy as these may be admitted under a different team)
Initial assessment
History
There are three main categories of patients who sustain ankle fractures:
- Fit and healthy patients
- More frail patients with osteoporosis
- Patients with diabetes or another peripheral neuropathy
For the fit and healthy patients, the clerking is very quick. The mechanism is usually a twist playing contact sports or a simple slip down a step. Time of injury and occupation are important to note.
Frail patients are much more complex and a thorough medical clerking is required including an extensive medication, social and mobility history. Remember to evaluate for medical causes of a fall (the page on hip fractures has a fairly comprehensive guide to this type of clerking).
In the diabetic group, it’s important to know how long they have been diabetic, what medications they are on and if they have any co-morbidities associated with diabetes i.e neuropathy, vascular disease, previous amputations (these factors have a big influence on management).
As always, if the ankle fracture is in the context of major trauma, perform an ATLS assessment.
Examination
First inspect the foot and ankle. Is there visible deformity? What does the skin look like? Are there any ulcers or open wounds? Even a pinprick is technically an open fracture, if it communicates with the joint. Look specifically at the medial side. Is there any bruising or swelling that could indicate a medial ligament injury?
Next, palpate for bony tenderness. Specifically, feel medially (medial malleolus and just distal, where the deltoid ligament runs), laterally (over the distal fibula and just anterior, posterior and inferior, where the ligaments attach) and proximally (over the proximal fibula).
Assuming this is an isolated injury, the neurovascular (NV) status of the limb and the soft tissues need to be assessed.
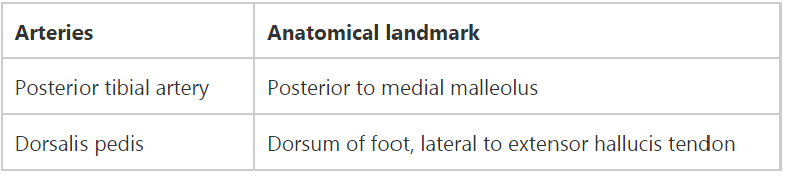
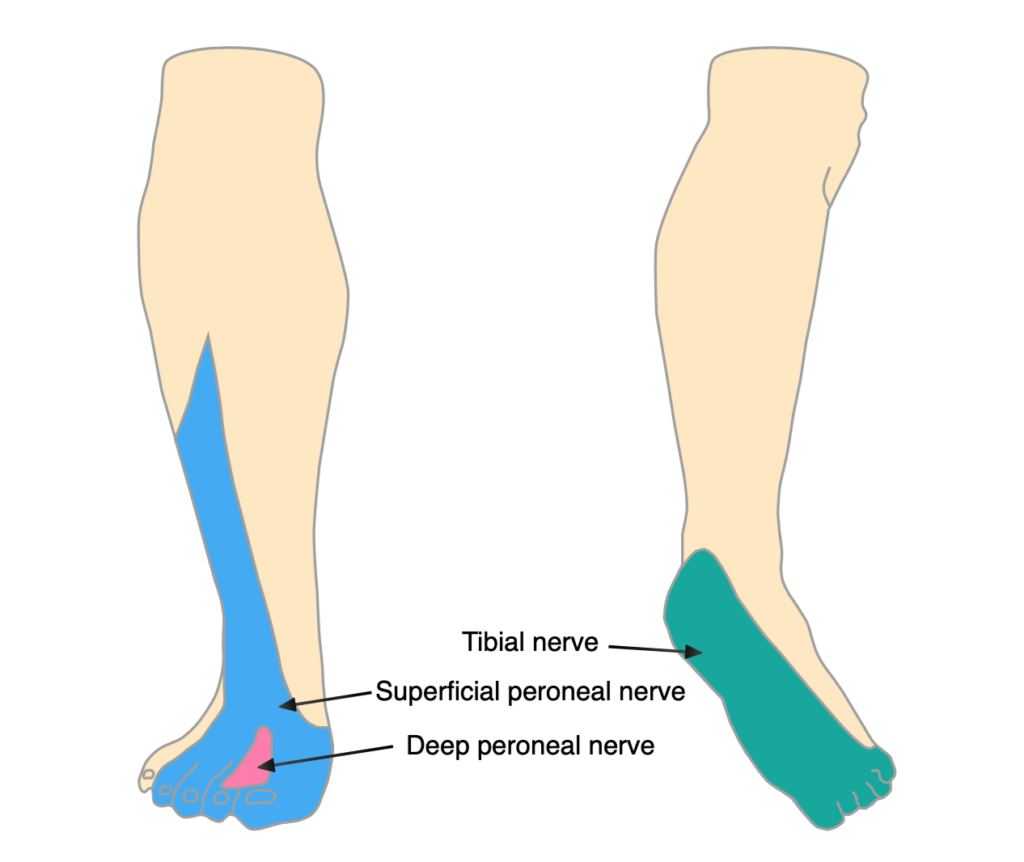
There are 3 nerves and 2 arteries that supply the foot and ankle. I find it useful to document them in a table so its absolutely clear to everyone who reads it. Patients won’t be able to evert their ankle, but they can all dorsi- and plantarflex their toes:
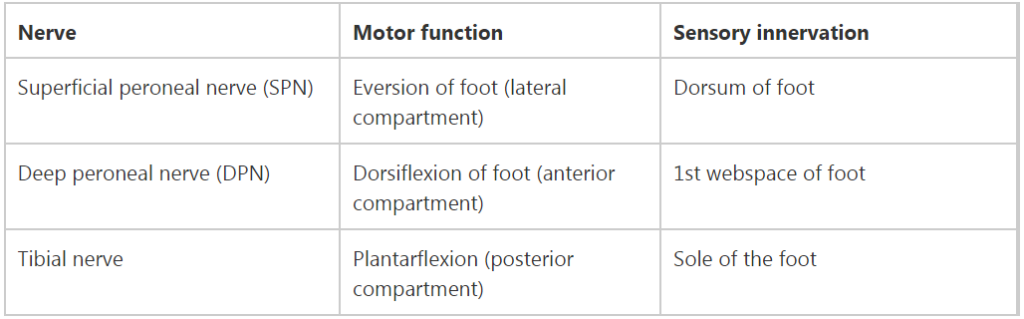
Document also the colour of the foot, its temperature and capillary refil – if the foot is ischaemic, call for help urgently!
Documentation of the soft tissues is vital. In addition, you can take a photo (with consent and using the appropriate format) that can be seen by the rest of the team in the morning trauma meeting. After 24 hours, most ankle fractures will be too swollen to operate on. It then takes 7-10 days for swelling to subside with the patient in bed with their leg elevated.
Note of caution: With ‘isolated’ medial malleolar or ‘isolated’ syndesmostic injuries, always examine the the proximal fibula to look for a Maisonneuve fractures (see classification section for further details). Equally, if ED refer a ‘isolated’ proximal fibula fracture, make sure to examine the patients ankle for a medial sided injury (this may be bony or ligamentous).

Initial management
Make sure the patient has been adequately resuscitated (A, B, C and D come before E)!
If there is an open fracture, manage as for any open fracture (see here).
The ankle joint must be reduced. This is non-negotiable in the majority of cases. See below for advice on reduction.
Once the above are complete, you must complete seven tasks/decisions, which must all be documented in the notes:
- Choice of splint
- Weight bearing status
- Analgesia
- Elevation
- Thromboprohylaxis
- Baseline/pre-theatre investigations
- Admission/discharge and follow up
Splinting
For stable fractures, patients can be placed into a fixed ankle boot and discharged with fracture clinical follow up or advice (depending on local protocol) – you’ll probably never get these referrals as ED are good at sorting them. They can potentially fully weight bear as pain allows, but if in doubt err on the side of caution and make the patient non-weight-bearing (NWB).
For unstable undisplaced fractures, patients are placed into a backslab with the foot in plantigrade (90 degrees of dorsiflexion). They then require a check XR in cast and a repeat NV exam. Keep NWB.
For unstable displaced or subluxed fractures, patients require immediate reduction (see section below) in ED, should be placed into a backslab and then a need post reduction XR and NV exam. Keep NWB.
Thromboprophylaxis
Assess DVT risk as per your local hospital policy. Most patients who are NWB in a cast/backslab need chemical thromboprophylaxis unless there are contra-indications.
Analgesia
Ankle fractures are painful and patients will require analgesia as per the WHO analgesia ladder. Majority will need paracetamol and codeine/tramadol. Avoid regular use of non-steroidals, as these may increase the chance of non-union.
Elevation
All patients admitted with an ankle fracture must have strict elevation overnight to the level of the heart. This can be achieved by multiple pillows or with manipulation of the hospital bed. It often falls on you to make sure this happens – DO NOT rely on the overnight ward staff to do this.
Any patient discharged with an ankle fracture should be given advice to strictly elevate. This means that unless they are mobilising, they should be laid flat with their ankle above the level of the heart.
Baseline/pre-theatre investigations
Use your common sense. A young fit patient with no cardiovascular history or exercise limitations does not routinely need further investigations. Any patient with comorbidities should have an ECG and baseline bloods (FBC, U&E, clotting if anticoagulated) if they are being admitted or are likely to require surgery. A CXR should be arranged for anyone who is having surgery and has a history of respiratory disease or shortness of breath on exertion.
Admission/discharge and follow up
See the relevant section below for advice on admission and discharge.
For any patient being discharged, make sure appropriate follow-up is arranged, usually in fracture clinic. If a patient is not being followed up (if your trust, for example, does not routinely follow up stable, undisplaced ankle fractures), make sure the patient knows this, and knows where to seek help if they need it. If a patient is from another area, and is going to return home to arrange their own follow-up, make sure they know to do this themselves.
Imaging and classification
Imaging
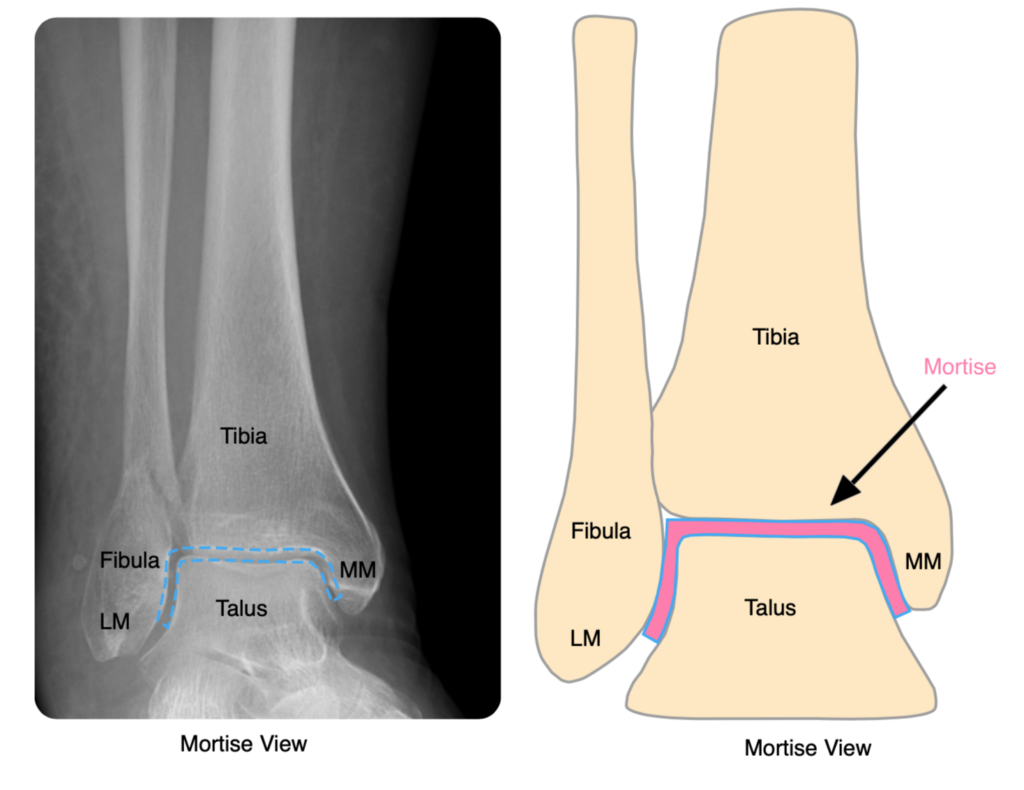
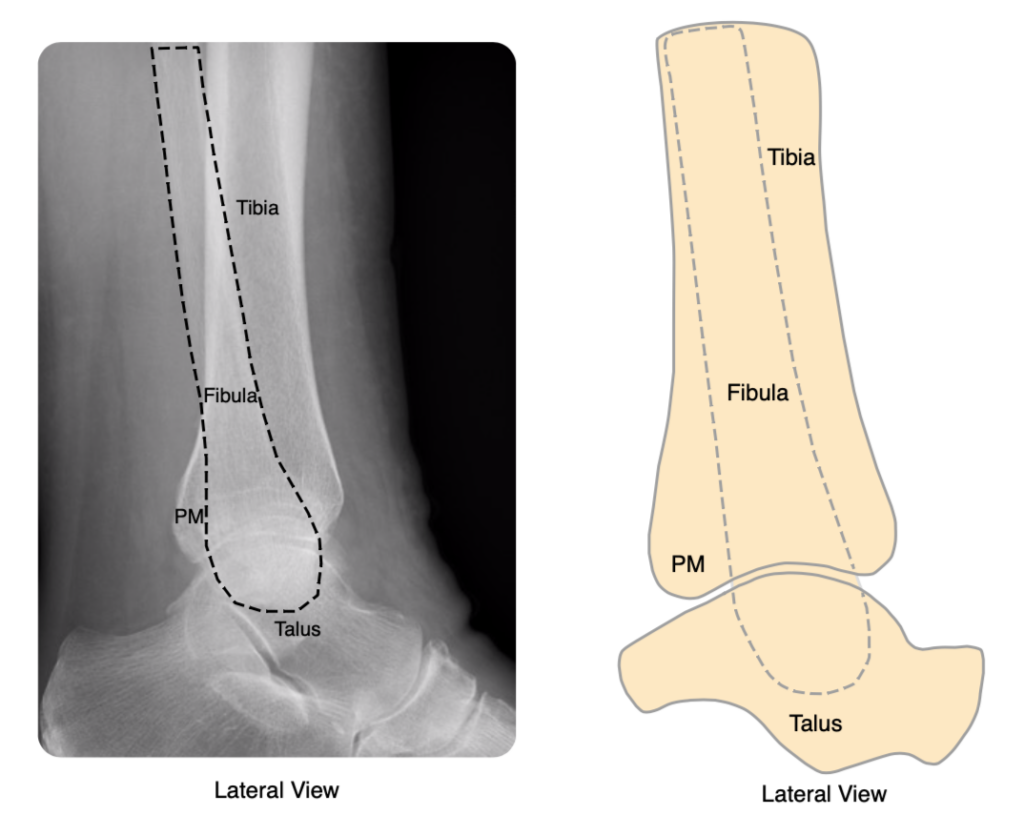
All patients require a mortise view (AP with 15 degrees of internal rotation) and lateral of the ankle:
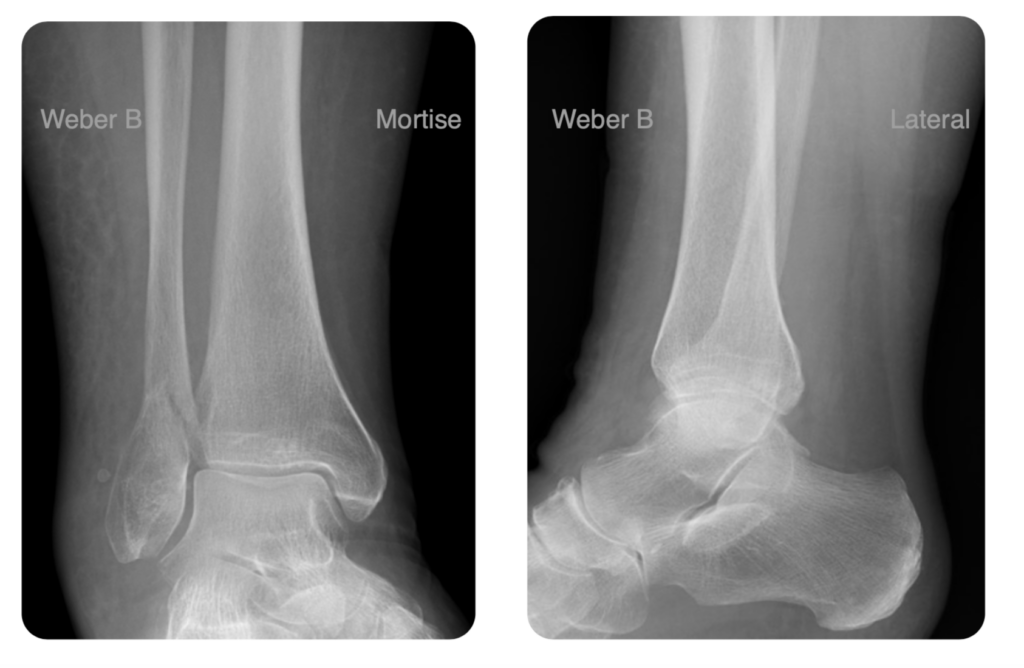
If a patient has an isolated Weber B fracture, with a congruent mortise, a weight-bearing XR is very helpful to determine stability – if the mortise remains congruent, with no talar tilt or shift, then the ankle is stable. Imaging departments may not be able to perform these overnight, however, and patients may be too painful, so if these are not available, treat the ankle as unstable and keep the patient NWB.
BOAST guidelines suggest considering CT imaging for “complex fracture patterns, particularly when there is a posterior malleolar fracture”. It is helpful to obtain these in the emergency department if they are indicated, but again they are often unavailable overnight. When requesting, the reason is for surgical planning: the location (posteromedial/posterolateral) makes a big difference, as does comminution and the presence of depressed or blocking fragments.
Classification
There are three major classifications to be aware of. These are not used in isolation, and the most thorough way of describing an injury is to combine all three (e.g. a bimalleolar, supination external rotation injury, with a Weber B fibular fracture). The Lauge-Hansen classification is not simple, however, and most people stick to the anatomical and Weber classifications.
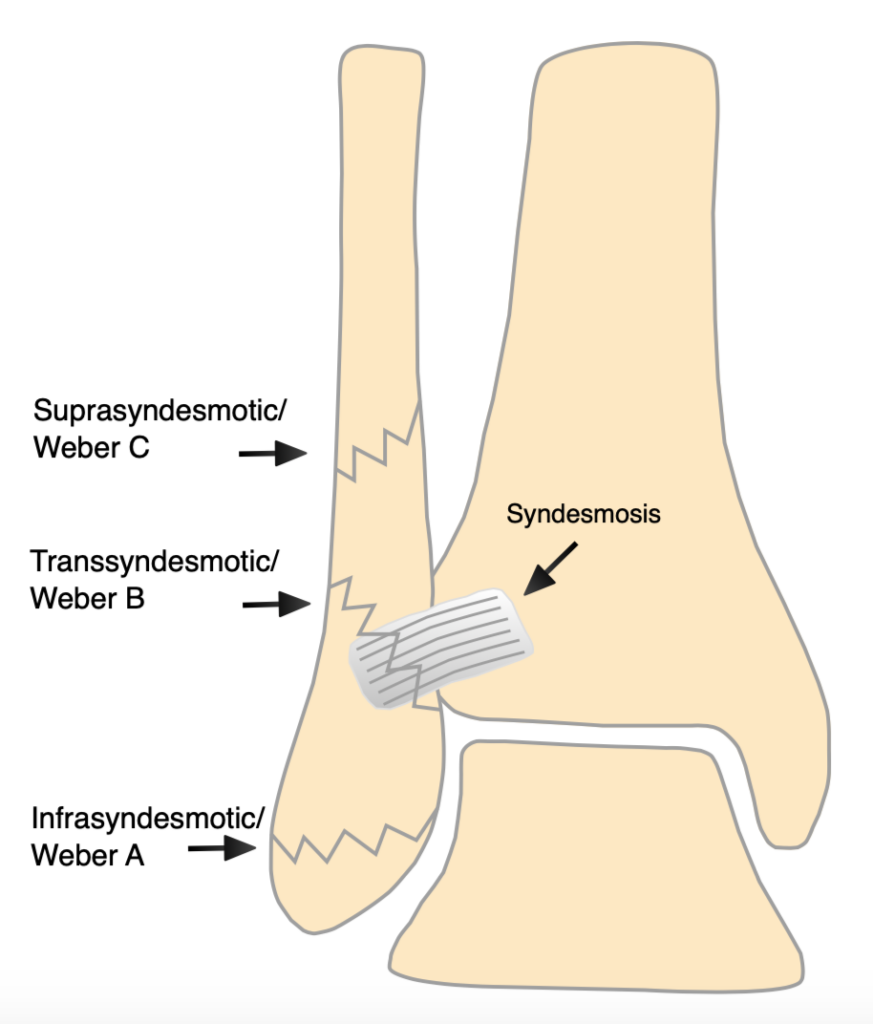
Anatomical (number of malleoli involved). There are three malleoli of the ankle: lateral (i.e. distal fibula), medial (the distal medial tibia) and posterior (the posterior rim of the distal tibia). Fractures can therefore be unimalleolar, bimalleolar or trimalleolar.
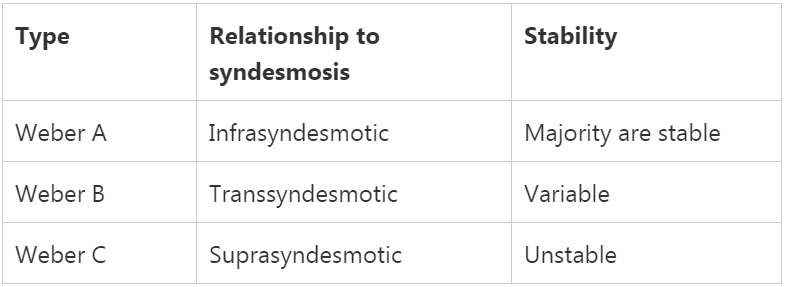
The Weber classification is based on the relationship of the distal fibular fracture to the syndesmosis:
The Lauge-Hansen classification is the most thorough and complex. It is not required knowledge of most SHOs, but if you understand this, then you understand more about ankle fractures than many orthopaedic surgeons! The best description and explanation I have found is here.
Stability and clinical anatomy
What makes an ankle fracture unstable?
Ankle fractures are a good example of the idiom that “a fracture is a soft tissue injury that happens to have an associated broken bone”. Whilst some fractures are unstable purely because of the broken bone, most stability is due to the integrity or otherwise of the ligaments.
A fracture may be unstable due to one or both:
- Medial ligament injury or avulsion fracture
- Syndesmosis injury (Weber C fractures almost invariably involve a syndesmosis injury)
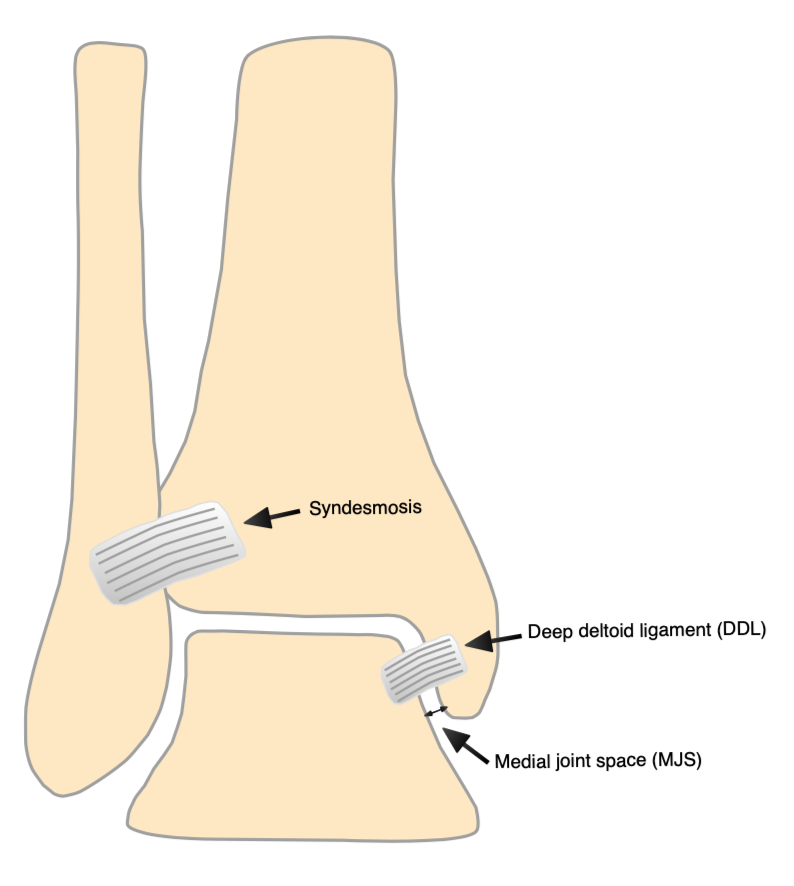
Assessing the medial ligamentous structures
Historically, great weight was placed on clinical examination of the medial side: bruising, swelling and tenderness were taken as markers of ligament injury, which might suggest surgery. Research has shown, however, that this is neither sensitive nor specific. Radiographic assessment, especially of weight-bearing XRs, is more commonly used currently.
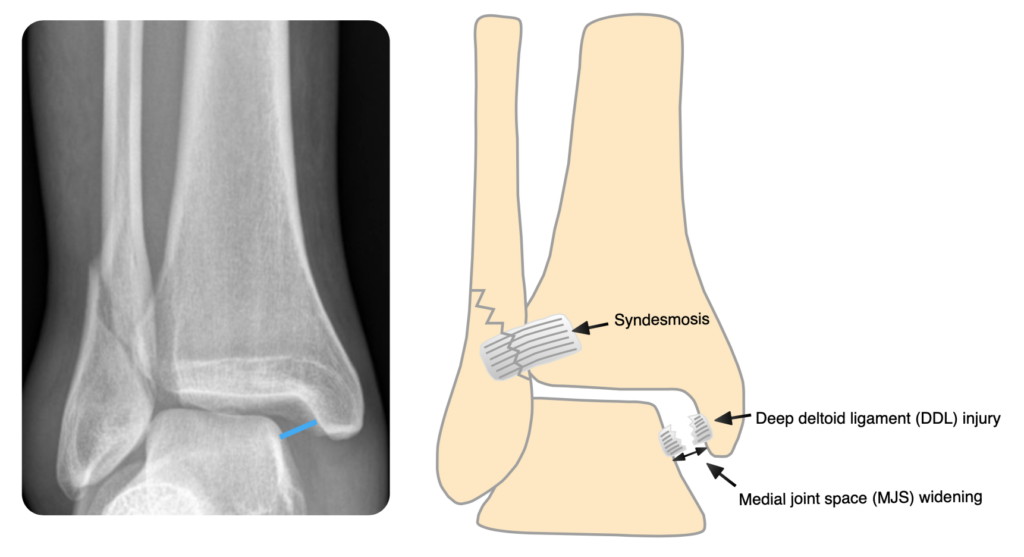
If there is a medial malleolar fracture, then the deltoid ligament is almost certainly non-functional and the ankle is likely to be unstable. In the absence of a fracture, look for talar tilt or shift (the talus should be directly under the tibia, and the talar and distal tibial articular surfaces should be parallel; if not, there is tilt and/or shift) and for widening of the medial joint space (the medial, superior and lateral joint spaces should all be equal):
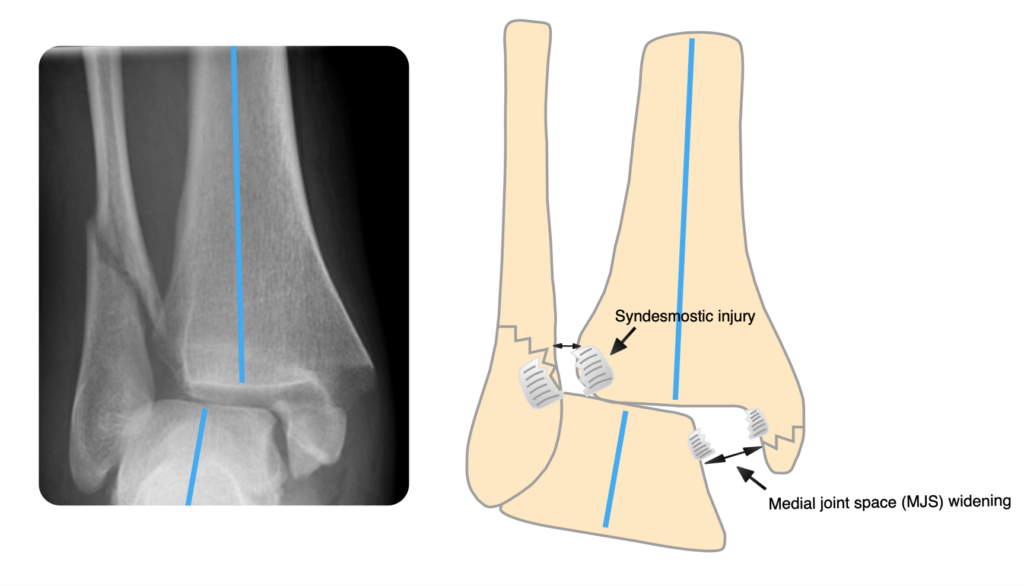
Assessing the syndesmosis
Look for talar shift/tilt (see above) or widening of the syndesmosis:
Pitfall
When the foot is in equinus (plantarflexion) the deep deltoid ligament (DDL) is lax and you may think there is some subtle medial joint space widening. When the foot is in plantigrade (foot is at 90 degrees of dorsiflexion) the DDL is tight (medial malleolus hugs the talus). In this situation, standing XRs are really useful. When you stand the foot is plantigrade and the DDL is tight – if there is MJS widening in this position, you know the fracture is definitely unstable.
Stable fractures
In general, the features of a stable fracture are:
- No medial joint space widening or talar shift/tilt
- No medial bruising/tenderness (but see note above)
- < 2mm displacement at fracture site
- Fracture in 1 place only (uni-malleolar)
Stable fractures include:
- Unimalleolar Weber A (infrasyndesmotic)
- Majority of isolated Weber B (transsyndemotic)
- Isolated undisplaced medial or posterior malleolar
If Weber A or B fractures are part of a bi or trimalleolar fracture pattern, they are unstable.
Unstable fractures
In general, features of an unstable fracture are:
- Multiple fractures
- Fractures above the syndesmosis
- Talar shift/tilt
- Medial joint space widening
- Open or high energy injury
Unstable fractures include:
- Uni-malleolar with features of instability
- Bi-malleolar
- Tri-malleolar
- Supra-syndesmotic (Weber C)
Reducing fractures in ED
N.B. The aim of this page is not to teach you to reduce fractures. You must ensure you are appropriately trained before performing any interventions. It is not possible to succinctly write a “guide to ankle fracture reduction” – every fracture is different and has its own ‘character’. We have provided some tips and tricks below for interest only.
N.B.2. The decision of whether or not a fracture needs reducing is entirely unrelated to whether or not it is going to need operative management. Once the fracture is reduced, the patient’s pain will improve as will their swelling and bruising. The tension is taken off neurovascular structures, and abnormal pressure on cartilage is relieved, reducing the risk of long-term arthritis. If there is a delay to surgery, it is better for the fragments to be well-aligned, so that soft tissues do not contract. Importantly, even fractures that appear terrible on admission, may be treated without an operation if they are well reduced in the emergency department. Do not accept “they’re going to need an operation anyway” as a reason not to reduce! This also applies to open fractures, where reducing the fracture (after removing any gross contamination) will reduce bacterial colonisation of the bones and fracture site.
Most importantly: unless a fracture is not reduced, the swelling will not go down, the patient is more likely to develop fracture blisters (see below), and in the worst case scenario, an initially closed fracture may become open due to skin ischaemia.

Deciding whether a fracture needs reducing
ED staff usually have a good understanding of which fractures need reducing, and which do not. As always, if you are unclear, discuss with a senior. Ultimately, the aim is for a congruent mortise view (talus under tibia, with parallel talus and distal tibia, and normal medial joint space) and lateral (no posterior subluxation of the talus). BEWARE: the mortise can look almost perfect and the ankle may be completely dislocated posteriorly!
Logistics of fracture reduction
As mentioned above, if you’re not confident in fracture reduction and haven’t been appropriately trained, you shouldn’t be doing it, but the following is a useful checklist:
Prepare
- Documented pre-reduction neurovascular status
- Verbal consent from patient
- 4 people (minimum): 1 to reduce, 1 to backslab (plaster technician if available or its YOU), sedation doctor (never try and sedate and reduce yourself), sedation/airway nurse
- Arrange transfer to resus for safe sedation
- Backslab ingredients: 2x 6 inch wool, 2x 6inch crepe bandage, 15cm and 10cm plaster of paris, tape, bucket of lukewarm water, aprons and gloves (it gets messy), block to put under thigh (or another assistant to support the thigh)
- If there is an open fracture: saline-soaked gauze and occlusive dressing
Perform
- Manipulate as required
- Wound dressing for open fracture
- Apply a backslab. NEVER put a full cast on a fresh ankle fracture
Check
- Re-check and document neurovascular status
- Arrange, review, and document result of check X-rays
Reduction techniques
As mentioned above: this is a technical procedure that you should not attempt without proper training. Every fracture is different, and you can make things significantly worse if you attempt reductions inappropriately.
Personally, I (HM) think that the best guide to ankle fracture reduction and splinting is in Charnley’s ‘Closed Treatment of Common Fractures‘, even though it was published in 1950!
Technique hints and tips
Most fractures are external rotation injuries, with lateral displacement of the talus. The tips below are aimed at these injuries.
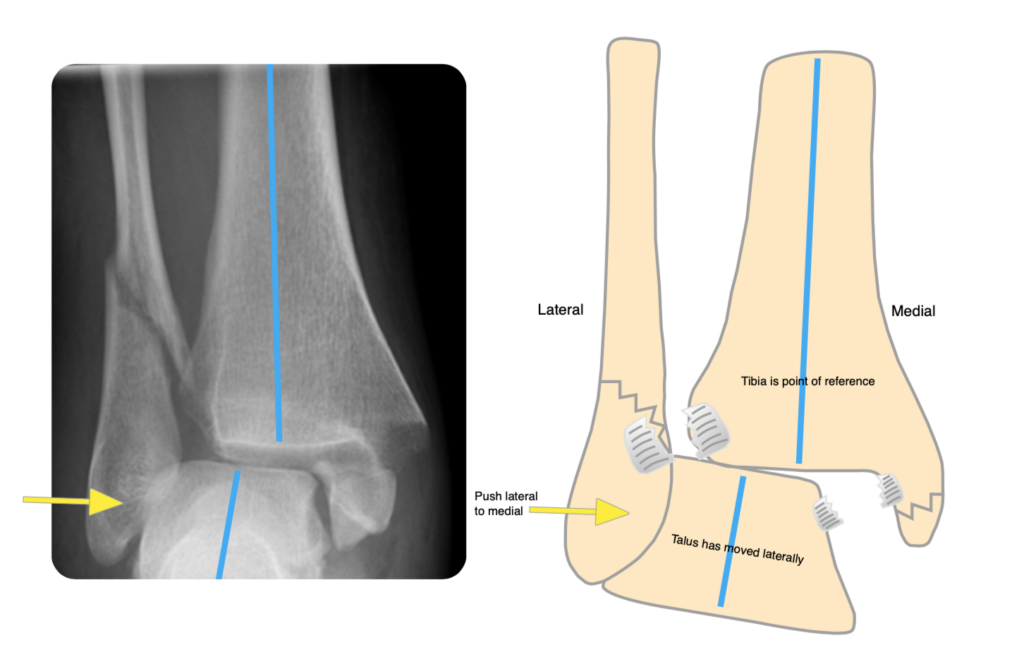
Due to the external rotation element, when the patient is lying in bed, the foot will point laterally. The talus may also be displaced posteriorly. Just by picking the foot up by the big toe, both of these will be corrected, and you will feel the joint reduce with a ‘clunk’. It is then just a case of applying a moulded backslab to reduce the fracture fully. Push lateral to medial: talus moves laterally (tibia is always point of reference).
Have one hand medially above the ankle and the other laterally just below the level of the ankle (if they are at the same level, nothing will move):
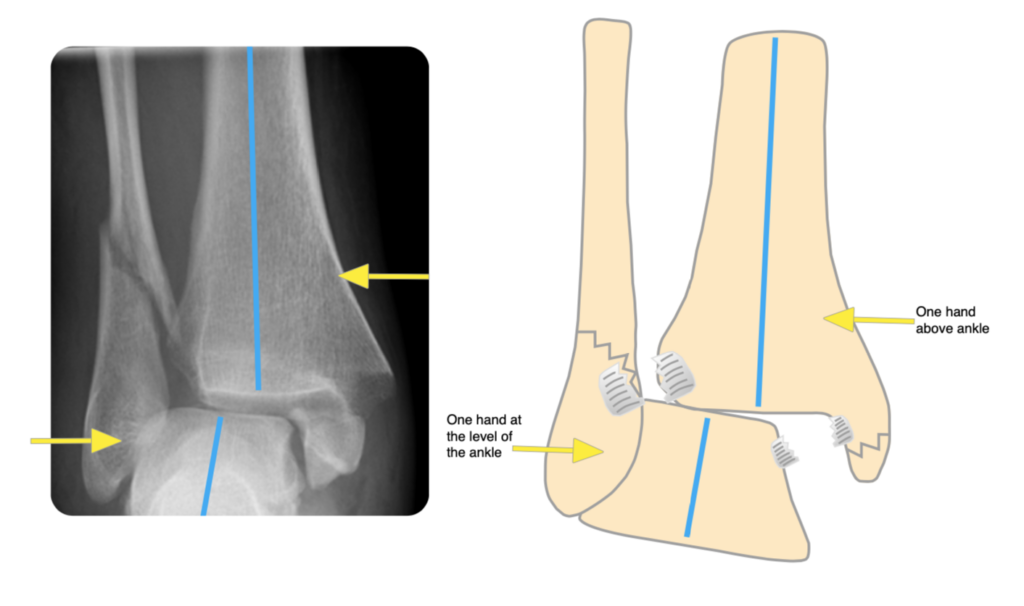
If there is a posterior malleolar fracture, you need to be pulling the heel forwards. This is achieved by having the distal (lateral) hand posteriorly. This is facilitated by externally rotating the entire leg.
Flex the knee: this relaxes the gastrocnemius (that crosses both the ankle & knee) and allows for an easier reduction. Having a block behind the thigh, or an assistant supporting the thigh, makes this a lot easier.
Push lateral to medial: talus moves laterally to end up underneath the tibia.
Make sure the ankle is at 90 degrees (plantigrade) in the backslab. It is vital that the ankle is in this position whilst all parts of the backslab (including the wool) are applied. Do not try and push the ankle into plantigrade if you have applied a backslab in plantarflexion: not only will you weaken the plaster, but there is a risk of causing pressure sores.
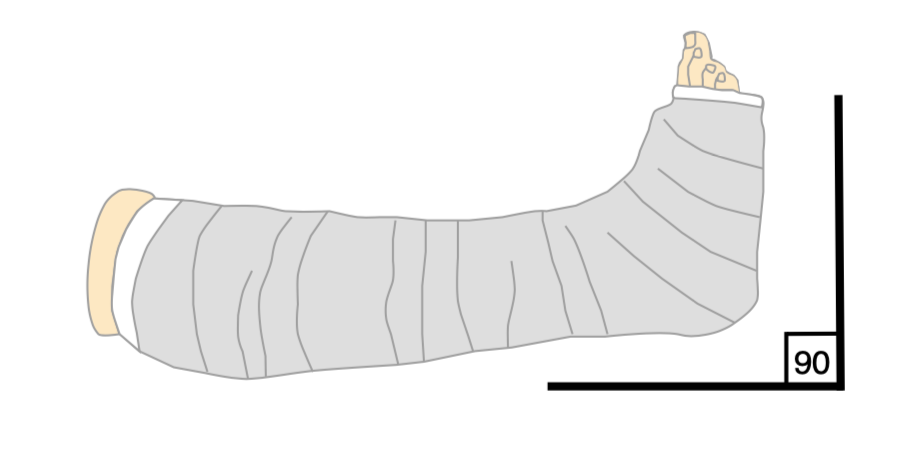
Take great care when applying any backslab or plaster to carefully pad any pressure points and to prevent direct contact of plaster on skin. Failure to do so can lead to disastrous pressure sores.
Admission, discharge and calling a senior
Always err on the side of caution: it is easy to discharge a patient, but much harder to bring them back into hospital, and by the time the mistake has been realised, harm may have occurred!
Who to admit:
- Unstable fractures that require surgery (there maybe no space on the next day trauma list but there are always cancellations and its easier to discharge them in the morning rather than re-admitting)
- Open fractures (if you are an orthoplastic centre; otherwise, they should be transferred from ED to your local referral centre)
- Social admissions – again check your hospital policy, the medical team may take them
When to call a senior urgently
- When you need help reducing a fracture. DO NOT let dislocated, subluxed or ankles with talar shift go to the ward (and definitely not home) without calling your senior (this happens quite frequently and there are no facilities on the ward to help with reductions)
- Any open fractures unless you are entirely happy with managing these in ED and arranging transfer to your local orthoplastic centre
- Any fracture with a persisting or new neurovascular deficit after reduction
Checklist
- Full clerking history (mechanism, timing, drug and social history) documented
- Examination: NV & soft tissues (photo if possible) documented
- Fracture reduced if required and appropriate immobilisation applied
- Weight bearing status documented (if unsure, keep NWB)
- Analgesia prescribed/provided
- Thromboprophylaxis prescribed
- Mark and consent patient if required (if you have experience and are happy doing it, otherwise the reg will do this in the morning)
- Radiology: XRs pre and post backslab. CT arranged if indicated
- ELEVATION arranged and checked. Advice on elevation if discharging (ideally with an advice leaflet)
- Keep the patient Nil by mouth with appropriate IV fluids if necessary (no food from 2am, water until 6am)
Definitive management
Most ankle fractures and almost all stable fractures are managed nonoperatively, with a cast or boot, with or without a period of non-weight-bearing. For very unstable fractures, in patients who are not suitable for internal fixation, a cast may be applied under anaesthetic (manipulation under anaesthetic, or MUA). There is some evidence that in the elderly, a specific type of cast, applied with a general anaesthetic, may be as good as internal fixation, even for unstable fractures.
There are hundreds of ways to treat ankle fractures surgically so don’t get bogged down in the detail. It is useful however to have some idea of the common fracture types and fixation methods.
It is vitally important that swelling is adequately reduced before internal fixation is applied. This may take many days! As mentioned above: if the ankle is not reduced, the swelling will not go down. If it is impossible to hold the ankle reduced in a backslab, then an external fixator may be required:

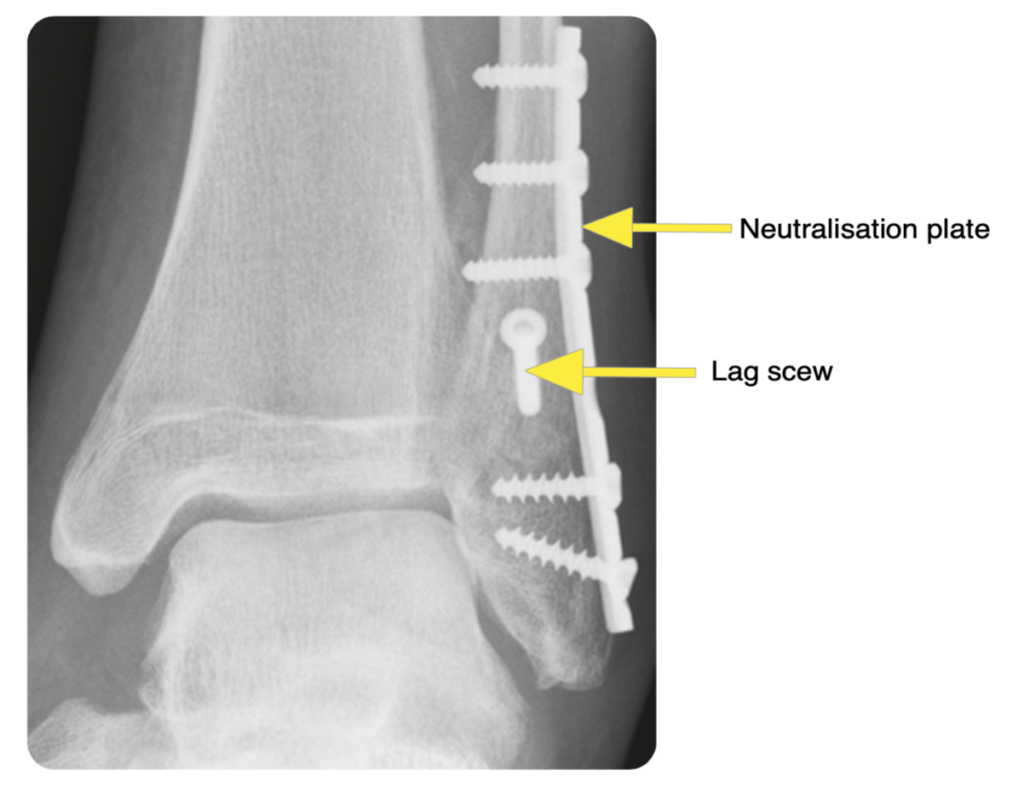
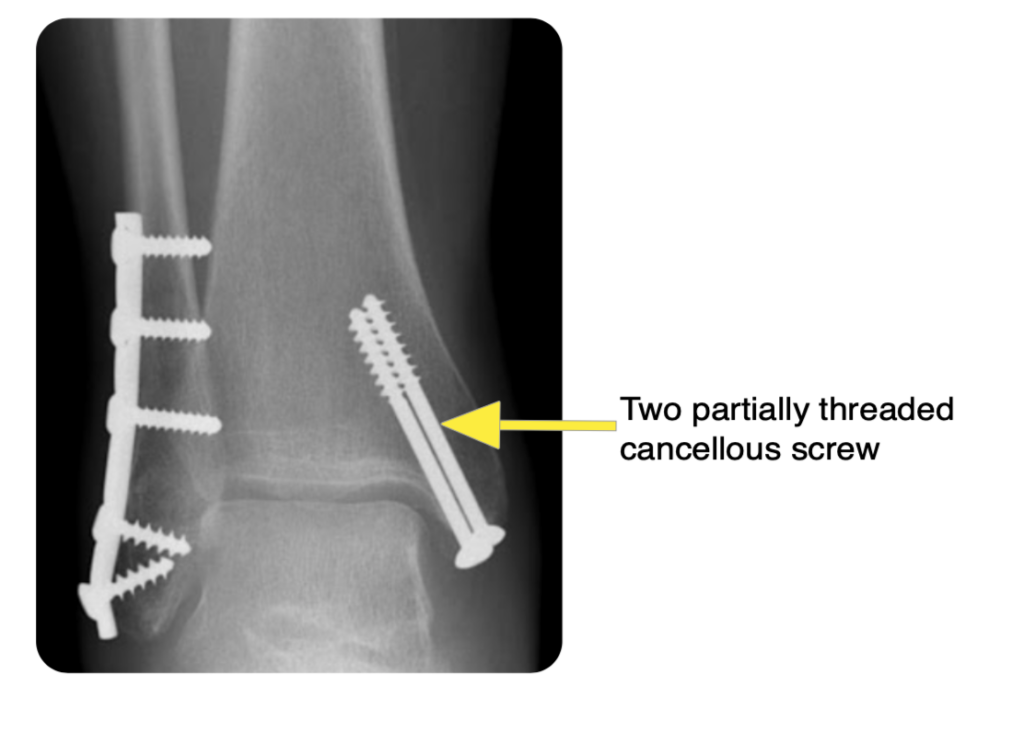
Unstable fractures are often managed with open reduction and internal fixation (ORIF).
The principles are to restore the ankle mortise and fibula length and to stabilise the syndesmosis. Depending on the fracture pattern, they are fixed with a combination of screws, plates, nails and tension band wires.
Common fracture patterns with common fixation methods:
Unstable Weber B: lag screw with neutralisation plate. Note that the deltoid is not commonly repaired: once the ankle is reduced, the ligament should heal (or at least scar tissue will form where it once was):
Displaced medial malleolus: partially threaded cancellous screws (other options include a plate, or tension band wire):
Syndesmotic injury: screws or tightropes
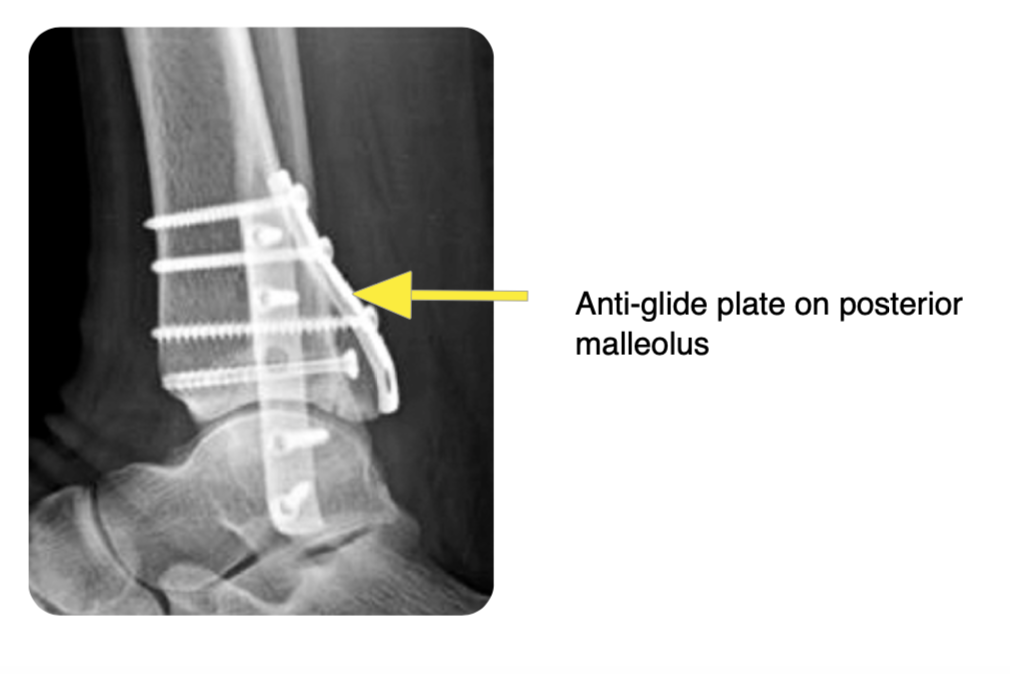
Posterior malleolar fractures may be fixed with screws alone, or with a posterior plate:
Guidelines
The BOAST guideline for the management of ankle fractures can be found here.
Page details
Author: Andrew Gardner
Editor: Hamish Macdonald
Last updated: 29/03/2020