Jump to
Admission, discharge and calling a senior
Overview
Fractures of the clavicle (collarbone) are generally managed non-operatively and do not need admission. Most will be reviewed in fracture clinic and will not need acute orthopaedic input, but it is important be be aware of the rare circumstances in which more urgent action is required.
Initial assessment
As always, these may be high-energy injuries, and it is important not to miss a life-threatening other injury – consider ATLS primary survey.
History
Document the mechanism and any other painful locations.
Due to the proximity of the neurovascular structures, ask about associated symptoms:
- Neuropathic pain/tingling in the arm and hand
- Numbness
- Weakness
- Severe distal pain
Examination
Assess the skin over the fracture site. Is there an open injury, or is the skin threatened? If the skin over the fracture is severely contused, stretched over the fracture, ischaemic (white) or necrotic (dark blue/black) then there is a risk of a closed fracture becoming open.
Document distal vascular status (brachial, radial and ulnar pulses, capillary refill).
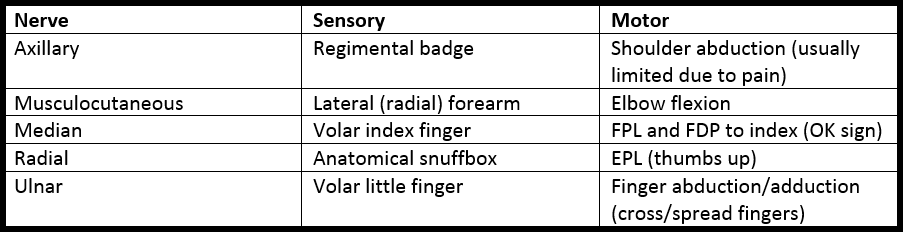
Document distal neurological function:
Initial management
Place into a broad-arm sling. Importantly, do not use a collar-and-cuff sling. The aim is to lift the lateral fragment up, reducing tension on the skin and soft tissues over the fracture apex and realigning the fracture somewhat. A collar-and-cuff lets the arm hang off the shoulder and will increase the deformity.
Checklist (for simple closed neurovascularly intact injury)
- Documented neurovascular examination
- Broad arm sling
- Fracture clinic appointment booked
Admission, discharge and calling a senior
Who to admit:
- Open fractures
- Fractures with threatened skin (i.e. which may become open imminently)
- Fractures with a neurovascular deficit
When to call the registrar urgently: if you’re considering admitting a clavicle fracture for any of the reasons described above
Imaging and classification
Imaging
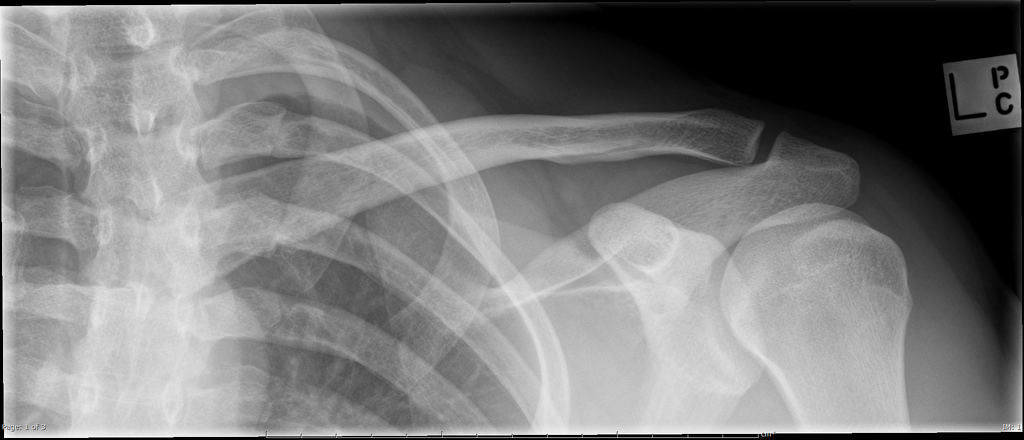
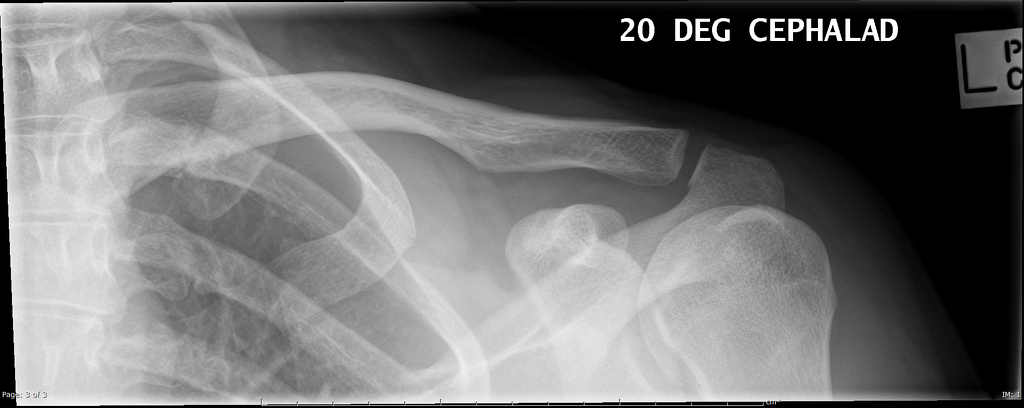
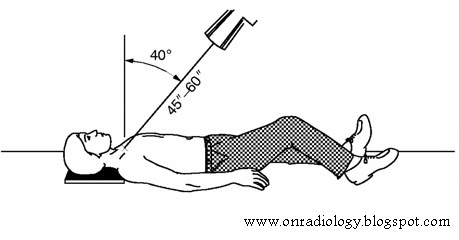
Plain radiographs are normally sufficient to diagnose this injury. Obtaining two orthogonal views without overlying structures obscuring the clavicle is tricky. The standard views are an AP and a 20 degree cephalad. The medial clavicle and SCJ are difficult to image, and a ‘serendipity view’ with 45 degrees of angulation may help (but CT is preferred).
Classification
Once more, the various classification systems do not necessarily influence your management, and it is most useful to describe the fracture in terms of location (medial 1/3, middle 1/3, lateral 1/3) and degree of comminution, angulation and displacement.
Definitive management
Non-operative
The majority of clavicle fractures are managed non-operatively, regardless of X-ray appearances. They are left in a broad-arm sling for 2-4 weeks (with regular removal from the sling for elbow ROM and shoulder pendulum exercises). Once pain and fracture crepitus settles, they can wean themselves out of the sling. X-rays at six weeks and thereafter until confirmed solid union, at which point contact sports can be resumed.
Operative
Decisions regarding operative fixation are controversial and vary between surgeons and hospitals. If indicated, fixation with an anterior or superior plate is normal. Relative indications for fixation include:
- Open fractures or threatened skin
- Neurovascular injury
- Simultaneous injury to the ipsilateral arm
- >2cm of clavicle shortening
- Patient preference (quicker return to function)
- Pain failing to settle following two weeks of conservative treatment
- Painful nonunion
- Some subtypes of distal 1/3 clavicle fractures
Page details
Author: Hamish Macdonald
Last updated: 29/03/2020