Jump to
Initial assessment and management
Admission, discharge and calling a senior
Overview
An open fracture is any bony injury that is open to the outside world. Injuries of the fingers and toes are managed slightly differently to other open fractures, so will have their own page. Remember, the ‘outside world’ includes hollow organs, so a pelvic fracture with a rectal injury, for example, should be managed as open.
Open fractures are high risk for morbidity and mortality, so treat them seriously.
Initial assessment and management
N.B. Elements of open fracture management are time critical, so your initial assessment and management should take place concurrently
N.B.2 Don’t be afraid to call for senior help early if you’re not happy with a situation/patient
N.B.3 These are often high energy injuries. An ATLS primary survey to identify and treat life-threatening illnesses should take place before management of the extremity injury (ABCD before E).
Take a focused history, using the AMPLE template (Allergies, Medications, Past medical history, Last ate, Events).
Obtain IV access and prescribe IV antibiotics as per your local hospital policy. This is a time-critical step and should be done as soon as you know the patient’s allergy status. It may even have been done by the ambulance crew.
Examine the limb:
- Skin and soft tissue injuries
- Distal neurovascular status (see separate page)
- Presence of compartment syndrome (see separate page)
Remove any ‘gross contamination’ (bits of dirt etc.) but do not perform a ‘mini-washout.
Take medical photographs of the limb with an approved device.
Reduce/realign the limb (obtain senior help if you are not able to do this).
Cover the wound with saline-soaked gauze and an occlusive dressing.
Splint the limb as appropriate.
Provide tetanus prophylaxis as per trust guidelines.
Check and document post-reduction neurovascular status.
Obtain post-reduction radiographs.
Perform a secondary survey to identify other injuries.
Stop, take a breather, and run through our checklist to make sure you haven’t missed anything!
Checklist
- AMPLE history documented
- IV antibiotics and tetanus prophylaxis given
- Initial examination documented
- Medical photographs recorded
- Gross contamination removed
- Limb realigned/fracture reduced
- Wound dressed appropriately
- Limb splinted appropriately
- Post-reduction neurovascular examination documented
- Post-reduction radiographs reviewed
- Secondary survey documented
- Location of definitive care determined and transfer/theatre/admission arranged as appropriate (see below)
Admission, discharge and calling a senior
Who to admit:
As a default, admit all open fractures unless transferring immediately to another hospital (see ‘location of care’ below. The management of open hand/forefoot injuries is discussed elsewhere; these are the only exceptions to a blanket “admit all” policy.
When to call a senior
Have a low threshold to call a senior, and do so immediately if:
- The patient needs urgent surgery (marine, farmyard or other gross contamination, arterial compromise, compartment syndrome)
- You are not able to reduce a fracture
- You think the patient needs urgent transfer, and are meeting resistance from the other hospital
- You don’t know whether the patient ought to be transferred
- You just don’t know what to do!
Definitive management
Location of care
According to BOAST/BAPRAS guidelines for open fractures excluding the hand, wrist and forefoot (see below): “patients with open fractures of long bones, hind foot or midfoot should be taken directly or transferred to a specialist centre that can provide orthoplastic* care. Patients with hand, wrist, forefoot or digit injuries may be managed locally following similar principles.” Orthoplastics is defined as: “a combined service of orthopaedic and plastic surgery consultants; sufficient combined operating lists with consultants from both specialties to meet the standards for timely management of open fractures; scheduled, combined review clinics for severe open fractures; specialist nursing teams able to care for both fractures and flaps.”
In reality, patients may be cared for in different locations depending on the exact setup of your local major trauma network. In our region all lower limb open fractures (excluding the forefoot) are managed in the major trauma unit, and are transferred directly from ED if they are not taken there directly by ambulance. The default for other open injuries is that they remain in the local trauma unit in the first instance, and are transferred only if there is a need for plastics input. This decision is usually made following consultant-to-consultant discussion.
Debridement
To prevent infection, debridement (i.e. removal of foreign material and dead tissue) and thorough washout must take place as early as safely possible. BOAST/BAPRAS guidelines state that this should occur:
- Immediately: highly contaminated wounds (e.g. agricultural, marine, sewage), arterial compromise or compartment syndrome
- Within 12hrs: other high energy open fractures
- Within 24hrs: other low energy open fractures
At the time of debridement, if the fracture is not able to be definitively stabilised, it will be stabilised temporarily with e.g. a splint, external or internal fixator.
Soft tissue coverage
The fracture has to be covered by soft tissue to heal without infection. This may be possible by ‘primary closure’ (i.e. closing the wounds directly) or may require regional or free flaps by the plastic surgeons. This coverage may take place at the time of first debridement or as a separate operation.
Definitive bony fixation
At the same time as soft tissue coverage is achieved, the fracture will be fixed as appropriate.
Classification
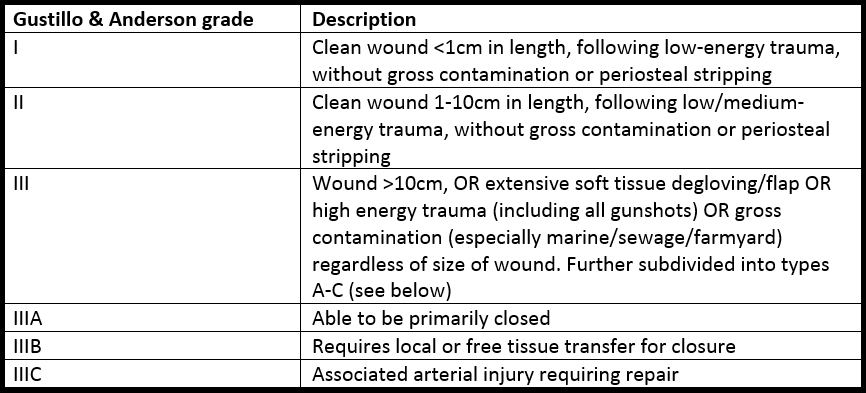
The most commonly used classification is that of Gustillo and Anderson, which was initially developed for tibial fractures and is only formally calculated after initial debridement, but is often used colloquially at presentation:
Guidelines
The BOAST/BAPRAS guidelines may be found here
Page details
Author: Hamish Macdonald
Last updated: 29/03/2020